Optimizing the Return-to-Sport Paradigm Following ACL Reconstruction (Part 1)
Jan 10, 2019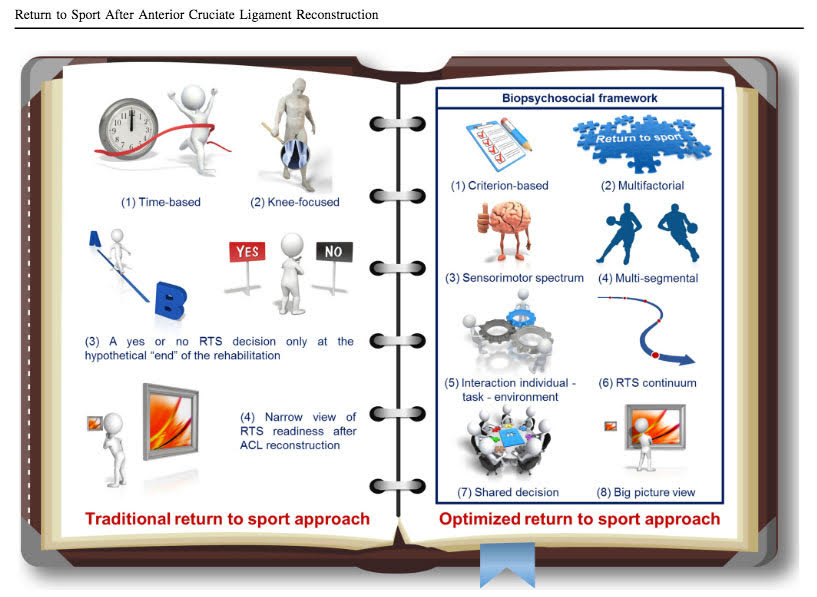
Here’s what we know:
- Secondary ACL injury risk after ACL reconstruction (ACLR) is approximately 15-23% (Wiggins 2016).
- Female soccer players after ACL reconstruction have 5x increased risk of new knee injuries than controls (Faltstrom 2018).
- 81% of athletes returned to some sort of sports, but only 65% returned to the pre-injury level of sport activity. 50% returned to competitive sports level (Ardern 2014).
- No gold standard exists for evaluating return-to-sport readiness after anterior cruciate ligament (ACL) reconstruction.
That last bullet point is a HUGE problem. How do we know when an athlete is ready?
Traditional return-to-sport criteria are mainly focused on the time after ACLR and knee-specific impairments, while the return-to-sport decision-making process is only made at the hypothetical “end” of the rehabilitation period. When is this “end” point? When the patient runs out of insurance-covered visits? When the ortho clears them based on a 5-minute exam? When there’s no longer a government shutdown? This “end” point is completely made up and very subjective. That is why we need more concrete, objective measures to allow these athletes return to sport at a high level with the lowest risk of re-injury.
Dingenen et al. proposes: “an optimized criterion-based continuous and multifactorial return-to-sport approach based on shared decision making, with a focus on a broad spectrum of individual sensorimotor and biomechanical outcomes, within a biopsychosocial framework.”
I could not agree more.
This means that we need to get away from time- and isolated-based assessments and look at this from a holistic 360 degree view, taking into account not only the biological factors of the athlete, but psychosocial factors as well. Since there are many individuals involved in this process, it takes a team to make the outcome truly successful. This team consists of the individual, their family, physical therapist, athletic trainer, orthopedic surgeon, sport coach, strength coach, etc.
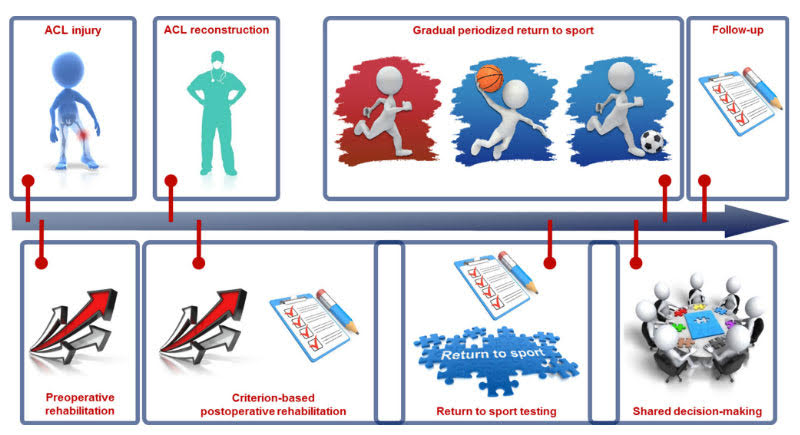
Remember – A single component alone (i.e. time) is not enough to determine whether someone is ready. All of the components below could have the box checked except the last one and this athlete would still not be ready. I hope this provides some insight to you if you are going through this process as an athlete, parent, or clinician looking to return to sport.
- Time: > 9 months after ACLR.
- Patient-Reported Outcome Measures: IKDC2000, Tegner Activity Scale, ACL-RSI, K-SES.
- Clinical Exam: Full range of motion, no pain, swelling, or laxity.
- Muscle Strength: Pivoting, contact, competitive sports (>100% limb symmetry index); non-pivoting, non-contact, recreational sports (>90% limb symmetry index).
- Hop Tests: Multi-directional (90% limb symmetry index).
- Assessment of Movement Quality: Multi-segment movement quality with and without fatigue
- Task and Environmental Constraints: Gradual progression of controlled tasks and environments to progressive, uncontrolled tasks and environments to replicate sport.
- Medical and Sport Risk Modifiers: Age, sex, personal medical history, type of sport, level of sport, position played, ability to protect (e.g. taping/bracing).
- Decision Modifiers: Timing of the season, external pressure from club, trainers, parents, conflict of interest (e.g. financial), lifestyle changes, priorities.
- Psychological Factors: This one is commonly overlooked – that is why next week, we will dive deeper into psychological readiness and how we can make sure this becomes just as important as the physical component of ACL rehab and performance.
Cheers,
Dr. Ravi
Source: Dingenen B, Gokeler A. Optimization of the Return-to-Sport Paradigm After Anterior Cruciate Ligament Reconstruction: A Critical Step Back to Move Forward. Sports Med. 2017;47(8):1487-1500.
Let us help you figure out to live your best active life today!
Remember, Movement is Medicine!

